- Dental Implants
- Bone Ridge Augmentation
- Surgical Extraction of Impacted Teeth
- Exposing Impacted Teeth for Orthodontic Treatment
- Biopsies of Soft and Hard Tissue in the Oral Cavity and the Face
- Surgical Treatment of Patients with Complex Medical Backgrounds
- Treating Patients with problems in the Joints and Muscles of the Masticatory (Chewing) System
- Surgical Procedures Using “Laughing Gas” (Nitrous Oxide), General Anaesthesia and Sedation
Dental Implants
Our teeth are an important factor in various functionalities, including talking and chewing, as well as aesthetics. The crown, which is the visible part of the tooth, is covered by hard enamel that is able to withstand the pressure of chewing and tearing food. The root of the tooth is composed of dentin. It is embedded in the jawbone and is normally not visible. The bone that envelopes the roots of the teeth is what holds them in place.
Sometimes, as part of an overall treatment plan, teeth need to be extracted. There are many reasons for extracting teeth, including crowded dentitions, various pathological processes, and infections in parts of the teeth and the surrounding tissue.
Dental implants replace the roots of the tooth and are inserted into the jawbone where the teeth were extracted. The implants can be placed immediately after extracting the tooth, but usually, due to the amount and quality of the bone it can only be done several months later. Sometimes, when the tooth is extracted, the jawbone, which has been damaged by the same causes that necessitated the extraction, needs to be augmented in order to preserve the alveolar volume. After placing the implants in the jawbone and waiting several months for the bone to heal, giving the implants stability and the ability to withstand the strain, the prosthodontist (oral rehabilitation doctor) can build the crowns on top of the implants. Cooperation between the surgeon and the prosthodontist is crucial to the success of the entire treatment. In special cases, the crowns can be positioned on the same day the implants are inserted. Determining the location of the implants, their dimensions and the distribution of force they will need to withstand, while taking into account the patients' desires and abilities, is challenging and requires meticulous planning, using advanced technologies, such as 3D models, and vast professional experience.
Bone Ridge Augmentation
When the bone intended to receive implants is inferior in quantity or quality, the bone ridge needs to be augmented. This ensures that future rehabilitation has the optimum starting point.
An assessment of the volume of the missing bone and its proximity to other structures, such as the maxillary sinus cavity or the mandibular nerve, is performed in a clinical examination involving imaging. Computed tomography (CT) and cone beam computed tomography (CBCT) are two imaging technologies that provide excellent 3D data. However, sometimes standard dental x-rays, including periapical or panoramic images, are sufficient.
When augmenting a bone ridge, a longer waiting period is normally required, between 6-12 months before the rehabilitative phase may begin.
The bone used for the augmentation can be taken from various sources, including the patient's own body, bones from another living being that undergo special processing, synthetically produced bone-like material or biological matter that induces spontaneous bone generation. The success of the process depends on the patient's cooperation and careful collaboration between the surgeon and the rehabilitation doctor.
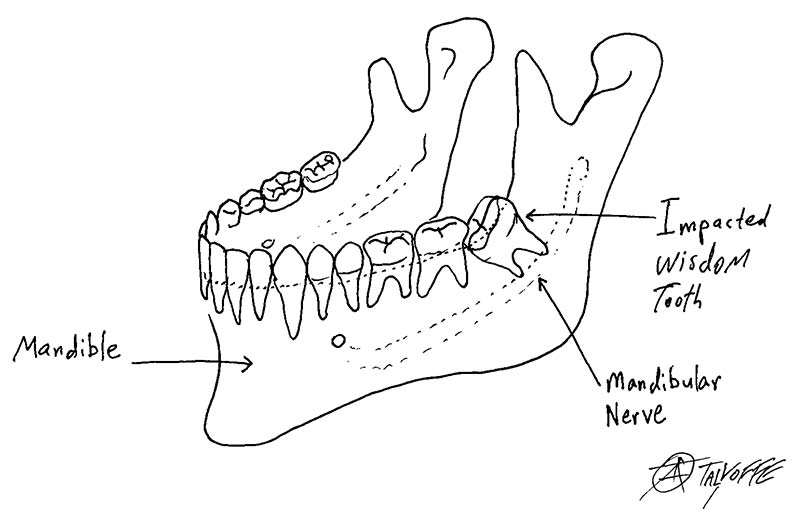
Surgical Extraction of Impacted Teeth
There are many reasons to extract teeth, including caries, gum problems, infections, crowded dentitions, supernumerary (redundant) teeth and impacted teeth.
Teeth that are fully impacted often do not need to be extracted. However, sometimes their presence can cause complications. For example, the dental sac that surrounds the crowns of the impacted teeth can enlarge and develop into a cyst that grows in a way that harms the jawbone and makes it thin and prone to fracture.
In addition, the presence of impacted or redundant teeth could interfere in orthodontic procedures. Partially impacted teeth are likely to cause more trouble than fully impacted teeth. Their partial impacted position means that the crown is exposed in the oral cavity, like the tip of an iceberg. The gums can grip the neck of the tooth, which is the part of the tooth between the crown and the root and is not coated by enamel, but cannot grip the enamel that covers the crown of the tooth, which is exposed to the oral cavity. This creates a pocket through which bacteria can penetrate the length of the tooth, causing chronic infection, which can lead to pain, damage to nearby teeth, swelling and unpleasant odours. The most common impacted teeth are wisdom teeth and canines. However, impacted and supernumerary teeth can occur in any jaw and anywhere teeth sprout.
Sometimes, impacted teeth are very close to important anatomical structures such as the lingual nerve, mandibular nerve or the maxillary sinus. In such cases, it is important to consult an oral and cranio-maxillofacial surgery specialist. Surgical extractions do not usually need to be performed in a hospital.
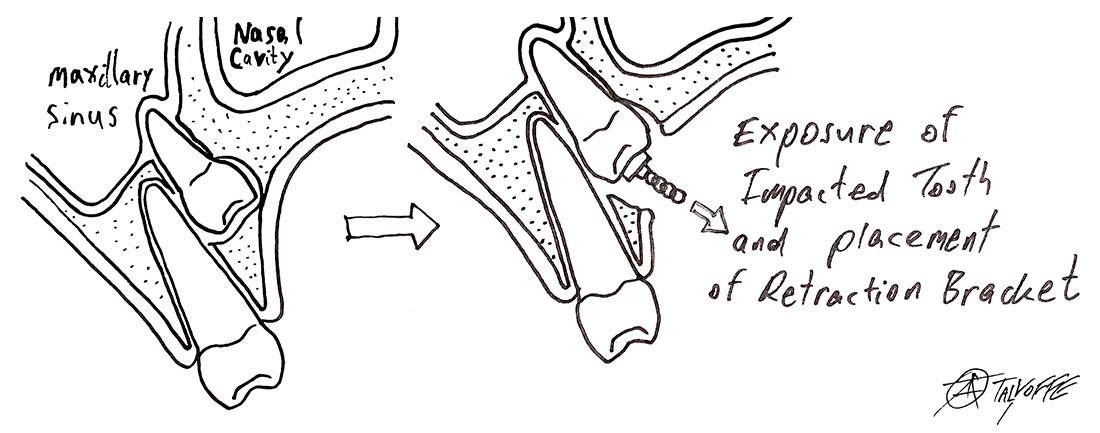
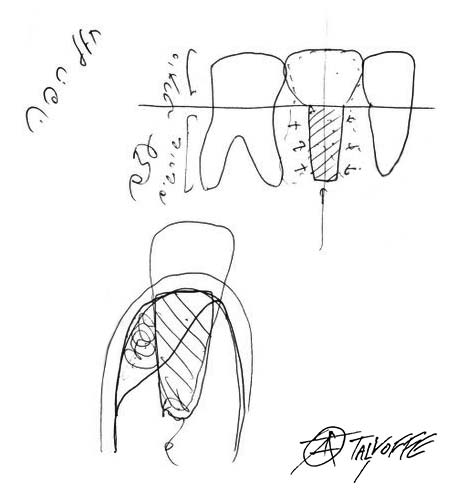
Exposing Impacted Teeth for Orthodontic Treatment
As part of an orthodontic treatment, sometimes impacted teeth need to be exposed to help them erupt into place. The teeth that need to be pulled into place could be impacted deep in the jaw, and exposing them requires skill and experience.
After exposing the impacted tooth, a bracket is bonded to its crown. A chain attached to the bracket is used to pull the tooth into the right direction until it reaches its proper place in the oral cavity.
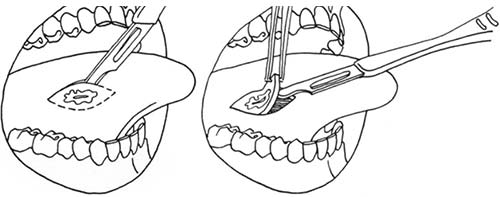
Biopsies of Soft and Hard Tissue in the Oral Cavity and the Face
When tissue in the face or the oral cavity is identified as being superfluous or out of place, has a different composition or looks abnormal; when a lesion does not heal or improve within a few days; or when imaging findings are suspicious; diagnostic surgery should be considered.
This procedure is called a biopsy. The word biopsy derives from the Greek bio, meaning life, and opsis, which means sight.
Head and neck cancer is the seventh most common type of cancer, and is affected by several risk factors, including smoking, alcohol consumption, bad oral hygiene, genetic predisposition and various viruses (HPV, EBV).
It is important to have an oral and maxillofacial surgeon periodically examine the mucous membranes of the oral cavity once you reach the age of 40.
If a biopsy has been taken, the sample will be examined under the microscope for diagnosis. Sometimes, treatment ends with the biopsy and no further steps are needed, and sometimes the biopsy is only the first step.

Surgical Treatment of Patients with Complex Medical Backgrounds
An important preliminary stage of any medical treatment in general and surgical procedures in particular is obtaining a thorough anamnesis (medical history) and understanding the full medical background of the patient, including their habits, medications, sensitivity to certain substances or drugs, past hospitalizations and previous surgical procedures.
Some background information will require special attention, such as cardiac or pulmonary conditions, oncological pasts, having received direct radiation to the head and neck area, imbalanced diabetes, poor renal function, and taking anticoagulants or platelet-aggregation inhibitors, drugs that interfere with the immunological response, or drugs that can delay or impact bone healing and remodelling, to name a few.
The older the patient is, the more likely they are to have one or more of these conditions, and a broad medical perspective is needed in order to suit the right treatment to the patient.

Treating Patients with problems in the Joints and Muscles of the Masticatory (Chewing) System
The lower jaw, the mandible, is classified as a long bone. Its frontal part, the body of the mandible, is shaped like a horseshoe that crosses the midline, and it holds the teeth. The two back parts—one on each side of the face—have perpendicular structures that end in ball-and-socket joints at the base of the skull, which are called the temporomandibular joints (TMJs). Each of these TMJs is a complex anatomical structure containing a cartilage disc located between the ball and the socket that is surrounded by a system of tendons, ligaments and muscles responsible for stabilizing and moving the mandible.
Symmetry – The TMJs serve as a growth centre of the mandible. If someone has minor differences in the length of their limbs, it usually causes no complications. However, such differences in the temporomandibular system are much more significant. In order for the chewing motion to take place, simultaneous action of the joints on both sides of the face is required. Minor discrepancies in the size of the joints could cause asymmetries that have considerable aesthetic and functional ramifications and could involve pain, noises when there is movement in the joints, malocclusion, the inability to open the mouth and a negative body image, with all that entails. During adolescence particularly, the development of facial asymmetry can have harmful psychological and social consequences.
Strain – The temporomandibular joints are held in place by a system of tendons, ligaments, cartilage and muscles that enable the various functions of the masticatory system, such as talking, chewing and swallowing.
It is a known fact that the left side of our face does not exactly mirror our right side and vice versa. On top of that, most of us do not chew our food equally in both sides of the mouth. We chew mostly in only one side, similar to our use of a dominant hand. Our posture, when awake, our body's position when sleeping, and clenching our teeth when we are awake and sleeping create asymmetrical strain on the TMJs. Our dental condition could also cause the distribution of the strain to be uneven. In addition, many people have para-functional habits, such as chewing gum, crushing ice or biting their fingernails. These can all cause damage in the form of the inability to open the mouth widely, pain, pressure, noises from the joints and from the muscles and ligaments that stabilise them, and asymmetry.
Joint Diseases – In addition to all of the above, like any other joint in the body, the TMJs are also susceptible to degenerative changes due to rheumatic joint diseases or autoimmune diseases, or as a result of infection, direct injury, tumours, degeneration caused by direct radiation, or disuse atrophy.
Treatment – The first step is conservative and involves reducing the strain on the joints by:
- Avoiding hard foods and opening the mouth to its widest;
- Avoiding para-functional habits (biting fingernails, chewing gum, etc.);
- Applying warm compresses;
- Fitting a rigid occlusal splint by a prosthodontics specialist;
- Using muscle relaxant drugs;
- Using anti-inflammatory and analgesic drugs.
If the conservative treatment is not appropriate to the clinical and imaging (Panorex, MRI, CT) findings, or if it is unsuccessful, we can move on to a surgical procedure:
- Arthrocentesis (joint drainage);
- Joint arthroscopy (keyhole surgery);
- Joint arthroplasty (open joint surgery).
If the mouth opening limitation is due to a muscular problem, or if there is malocclusion, physiotherapy that focuses on the masticatory (chewing) muscles should be considered.
Surgical Procedures Using “Laughing Gas” (Nitrous Oxide), General Anaesthesia and Sedation
When a patient suffers severe anxiety before a surgical procedure, or when full cooperation of the patient throughout the treatment cannot be guaranteed (for example, with children who need dental treatment), there are several methods that can be used to help complete the procedure:
Using laughing gas - A mixture of oxygen and nitrous oxide is inhaled through the nose and carefully monitored by the doctor. Special training is required before a dentist may administer nitrous oxide, and not every dentist is licensed to use it. Using nitrous oxide on pregnant women is prohibited. Laughing gas has practically no side effects, although patients might temporarily feel a little dizzy or nauseous after using it.
General anaesthesia and sedation - Technological advances and improved skills, combined with a rise in the demand to carry out several procedures at once, have also brought about an increase in using these methods. However, we must remember that they are not risk free. Using anaesthesia and sedation require the presence of an anaesthesiologist and a dentist with a special license from the Ministry of Health.